MAGGIO 2025
Chiropractic Rehabilitation for Adolescent Idiopathic Scoliosis: End-of-Growth and Skeletal Maturity Results
Abstract
The aim of this study was to evaluate the radiographic outcomes obtained in a sample of patients treated with a chiropractic scoliosis-specific exercise program for patients with adolescent idiopathic scoliosis. Patients were treated and subsequently followed through skeletal maturity, and their results were reported in accordance with the SOSORT Consensus Guidelines. A total of 60 patient charts were consecutively selected when they met inclusion criteria. Cobb angle measurements and Risser staging were collected on all images. Using SOSORT criteria, 51.7% of patients achieved curve correction and 38.3% achieved stabilization. In the curve correction group, average total correction was 12.75°. A small number of sampled patients’ curves progressed, with a 13% failure rate based upon patients who dropped out before skeletal maturity combined with those who had progressed at skeletal maturity. Future studies are needed to corroborate these observations.
Introduction
Adolescent idiopathic scoliosis is defined as a curvature of the spine with a Cobb angle of more than 10 degrees with concomitant rotational displacement.1 Curvatures larger than 50° at skeletal maturity are at high risk of continued progression throughout the lifespan.2 While bracing and surgical intervention have been the mainstays of conventional scoliosis management for progressive curvatures, exercise-based methods have become more known, with various exercise-based methods being published mainly from Europe.3,4
The main objectives of exercise treatment for idiopathic scoliosis to date have primarily been 3 outcomes5: i) decreased pain; ii) improved pulmonary function; and iii) preventing curve progression. Although it has been suggested that scoliosis exercises are unable to provide curve correction in adolescent cases,6 there are studies documenting the ability of scoliosis-specific exercises to alter the course of adolescent idiopathic scoliosis. In a review of manual therapy by Romano and Negrini,7 they found 3 studies that fit their criteria, all of which were low quality. Additionally, none of these 3 studies followed up with patients through skeletal maturity. Therefore, it is unknown how to best translate their conclusions into clinical practice.
Since the review by Romano and Negrini, subsequent randomized controlled trials, case reports and series have been published. A randomized controlled trial (RCT) by Monticone et al.8 assessed a treatment program consisting of active self-correction and task-oriented exercises. Using radiographic Cobb angle and the Health Related Quality of Life (HRQL) questionnaire, they showed statistically significant improvements in Cobb angle and quality of life. Another RCT by Kuru et al.9 showed Cobb angle changes in patients receiving clinic-based Schroth scoliosis therapy under physical therapist supervision. A third RCT by Schreiber et al.10 showed that patients participating in a scoliosis-specific exercise program in addition to standard of care management achieved statistically significant improvements in back muscle endurance, as well as self-rated pain and self-image scores on the Scoliosis Research Society (SRS-22r) questionnaire. The therapies in these studies were managed and/or supervised by physical therapists. Only 2 such subsequent reports were published by chiropractic authors. These studies followed adolescent patients to skeletal maturity or beyond 11,12 but in only 3 total patients. This study presents a larger data sample of patients with adolescent idiopathic scoliosis who were treated, discharged to home care, and followed up with through skeletal maturity. The results of this study are reported according to criteria previously described in the BrAIST study,13 as well as guidelines created by the Society on Spinal Orthopedic and Rehabilitation Treatment (SOSORT) and the Scoliosis Research Society (SRS) non-operative management committee.14
Materials and Methods
We conducted a power analysis using Power and Precision 4 software. Using a 95% confidence interval, as well as improvement of 6° as the target outcome, our analysis showed that we needed a sample size of at least 50 patients to make our outcome both clinically and statistically significant. We consecutively sampled patient charts from two separate chiropractic clinics if they met the following inclusion criteria: i) patient had a history of adolescent idiopathic scoliosis >10°; ii) initiated treatment at the chiropractic office between Risser 0-2; iii) were given home exercises to continue on their own; and iv) had at least one follow-up visit at end of growth, defined as a Risser 3/4, or at skeletal maturity, defined as Risser 5. Adhering to these inclusion criteria, a total of 60 patient charts were selected. Patients whose charts were selected gave their written informed consent for their information to the used. We applied for and received Institutional Review Board (IRB) exemption for this study through IntegReview IRB.
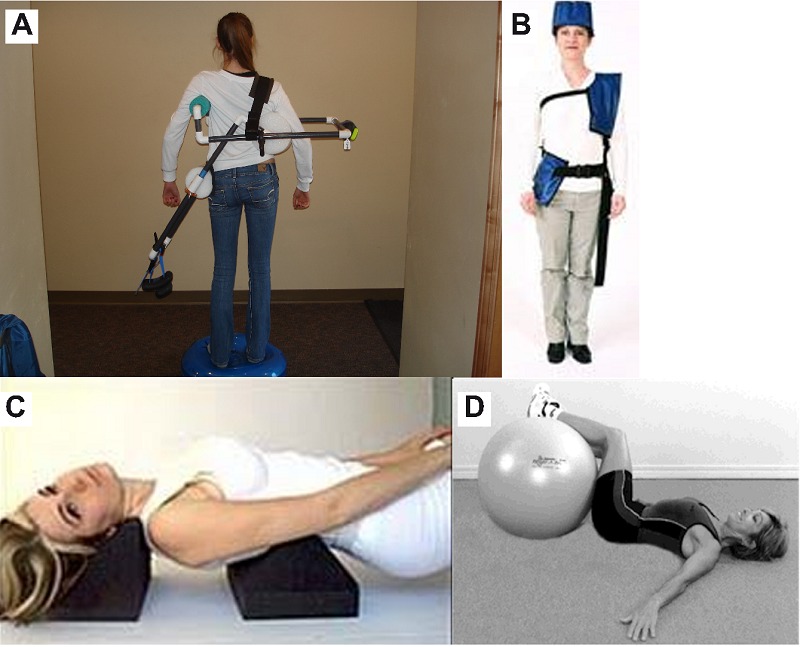
All patients had participated in a short-term chiropractic rehabilitation program. The treatment approach provided to the sample population takes advantage of central reflexive neuromotor control. In order to recruit these automatic postural control reflexes, external postural weighting was employed in various configurations, depending upon each patient’s curve pattern. These external postural weights purposely alter the centers of mass of the head, torso, and pelvis in specific vectors to cause automatic neuromuscular responses to counterbalance the external weight in predictable dimensions. Examples of this postural weighting process have been previously reported in scoliosis treatment.11,12,15 All patients in this study were prescribed their own sets of this weighting system for both in-office treatment as well as home use. Patients performed proprioceptive balancing on a 24-inch vestibular disc while using a cantilever exercise apparatus that increases the leverage of these externally placed postural weights without needing to add extra weight. By lengthening the distance of the weight from the patient’s torso, the leverage of said weight on the torso is increased. As patients progressed through care, many increased the difficulty of the exercise by performing this activity while balancing on the vestibular disc on top of a whole body vibration platform set at 30Hz. The goal of this therapy is to repetitively recruit reflexive postural muscle control while the patients perform a conscious activity (i.e., balancing on the vestibular disc), thus making the postural adaptations to the externally applied weight automatic, reflexive responses instead of voluntary muscle recruitment patterns such as those used in other types of scoliosis-specific exercise protocols.16
Motorized repetitive traction, supine positional traction, and chiropractic manipulation were administered to patients as well. Motorized repetitive traction was performed to decrease ligament hysteresis in concave paraspinal ligaments. Supine positional traction and related exercises were performed to promote a normal sagittal contour, providing a biomechanical baseline from which to perform specific core spinal stabilization excercises (Figure 1). Chiropractic manipulation was performed on patients when active range-of-motion restrictions were observed. Patients received an average of 1-3 manipulations over the 1-2 weeks of therapy. These therapies were organized and performed for each patient as his or her curve pattern dictated. They were performed for approximately 25 hours per each week of therapy. Upon discharge patients were given an individualized exercise prescription for home care to continue on an ongoing basis. Typical home exercise recommendations included two daily exercise sessions lasting 25-35 minutes each. Once they reached skeletal maturity a final evaluation was performed, and they were then dismissed from active management.
Figure 1.
Results
To be consistent with SOSORT/SRS14 and BrAIST13 criteria, we calculated the following outcomes: the percentage of patients who progressed beyond 50°, the percentage of patients who corrected 6° or more, the percentage who progressed 6° or more, and the percentage of patients whose curves stabilized at ±5° from the baseline measurement.
Under these criteria, successful treatment was observed in 90% of the entire cohort (defined as the total percent of patients who achieved curve correction or curve stabilization); 51.7% correction and 38.3% stabilization. In those patients who achieved curve correction, the average correction was 12.75°. The remaining 10% of patients had curve progression of 6° or more. Data for the entire cohort can be found in Table 1.
Table 1.
Data for the entire cohort of patients.
| Curve type | Age | TCobb1 | LCobb1 | Risser1 | TCobb2 | LCobb2 | Risser2 | Treatment time (yrs) | Fail |
|---|---|---|---|---|---|---|---|---|---|
| T | 11.8 | 24 | 1 | 8 | 4 | 4.67 | |||
| TL | 10.1 | 52 | 0 | 36 | 5 | 4.17 | |||
| T | 10.9 | 48 | 1 | 40 | 5 | 4.58 | |||
| T | 10.5 | 32 | 1 | 24 | 4 | 4.08 | |||
| TL | 12.3 | 24 | 2 | 12 | 5 | 4.33 | |||
| T | 13 | 20 | 2 | 11 | 5 | 4.83 | |||
| T | 11 | 42 | 1 | 30 | 5 | 6.17 | |||
| T | 11.3 | 24 | 1 | 14 | 4 | 5.25 | |||
| D | 12 | 79 | 71 | 1 | 78 | 66 | 5 | 4.58 | |
| D | 11 | 38 | 31 | 0 | 68 | 58 | 4 | 4.67 | Yes |
| T | 10.7 | 42 | 0 | 26 | 4 | 5.17 | |||
| D | 11.5 | 31 | 17 | 0 | 48 | 28 | 3 | 1.67 | Yes |
| TL | 13.3 | 35 | 2 | 17 | 5 | 4.08 | |||
| D | 12 | 59 | 37 | 1 | 53 | 33 | 5 | 4.17 | |
| TL | 12.5 | 24 | 1 | 18 | 4 | 3.08 | |||
| T | 11.9 | 29 | 1 | 20 | 4 | 2.5 | |||
| D | 13.5 | 26 | 24 | 3 | 15 | 9 | 5 | 2.08 | |
| T | 10.7 | 22 | 0 | 14 | 4 | 4.33 | |||
| D | 11.2 | 49 | 32 | 1 | 66 | 40 | 4 | 2.5 | Yes |
| D | 14.1 | 34 | 29 | 3 | 21 | 20 | 5 | 1.75 | |
| TL | 13 | 36 | 2 | 33 | 4 | 2.33 | |||
| L | 11.2 | 28 | 1 | 33 | 4 | 2.67 | |||
| D | 12.5 | 26 | 22 | 2 | 23 | 15 | 5 | 3.58 | |
| T | 12.2 | 19 | 2 | 8 | 4 | 2.08 | |||
| L | 11.7 | 29 | 2 | 20 | 4 | 1.67 | |||
| T | 12.5 | 28 | 2 | 27 | 4 | 2.17 | |||
| D | 11.2 | 35 | 32 | 1 | 23 | 19 | 4 | 3.83 | |
| TL | 12.1 | 27 | 1 | 31 | 4 | 2.92 | |||
| D | 10.5 | 24 | 36 | 1 | 27 | 32 | 3 | 1.25 | |
| TL | 11.7 | 36 | 1 | 29 | 4 | 2.25 | |||
| TL | 10.2 | 41 | 0 | 41 | 3 | 2.58 | |||
| D | 11.9 | 40 | 22 | 1 | 32 | 30 | 4 | 2.75 | |
| TL | 13.7 | 22 | 3 | 13 | 5 | 2.42 | |||
| D | 12.1 | 12 | 15 | 0 | 0 | 6 | 3 | 2.75 | |
| TL | 13.2 | 29 | 0 | 12 | 3 | 1.33 | |||
| T | 14 | 50 | 3 | 46 | 5 | 1.75 | |||
| TL | 14 | 38 | 2 | 22 | 5 | 3.33 | |||
| TL | 14 | 47 | 2 | 26 | 5 | 3.33 | |||
| T | 10.5 | 29 | 0 | 3 | 3 | 3.33 | |||
| L | 14.1 | 36 | 0 | 41 | 4 | 3.33 | |||
| D | 13.7 | 26 | 25 | 3 | 21 | 21 | 4 | 0.75 | |
| T | 13.2 | 25 | 2 | 23 | 4 | 1.25 | |||
| D | 13.2 | 51 | 48 | 3 | 49 | 43 | 5 | 1.75 | |
| D | 12.9 | 38 | 54 | 2 | 50 | 65 | 5 | 3.17 | Yes |
| TL | 12.9 | 24 | 1 | 28 | 4 | 1.75 | |||
| D | 12 | 20 | 16 | 0 | 12 | 8 | 4 | 2 | |
| D | 12.2 | 19 | 26 | 0 | 26 | 28 | 2 | 1.33 | * |
| D | 13.9 | 41 | 33 | 2 | 39 | 26 | 4 | 1.08 | |
| TL | 14.9 | 58 | 3 | 44 | 5 | 1.08 | |||
| D | 12.9 | 49 | 32 | 1 | 45 | 22 | 4 | 2.08 | |
| TL | 11.5 | 20 | 0 | 7 | 2 | 2.08 | * | ||
| TL | 11.5 | 18 | 2 | 14 | 4 | 1.25 | |||
| TL | 14 | 33 | 0 | 45 | 3 | 2.33 | Yes | ||
| D | 12.4 | 25 | 17 | 0 | 20 | 16 | 3 | 1.42 | |
| D | 11.8 | 58 | 48 | 1 | 58 | 48 | 5 | 2.33 | |
| D | 14 | 41 | 48 | 3 | 34 | 34 | 5 | 2.67 | |
| T | 13.7 | 31 | 1 | 30 | 4 | 1.67 | |||
| D | 13.1 | 29 | 23 | 1 | 25 | 25 | 4 | 1.17 | |
| D | 13 | 54 | 43 | 1 | 45 | 31 | 4 | 1.42 | |
| T | 10.7 | 44 | 0 | 39 | 1 | 1.42 | * | ||
| AVG | 12.31 | 34.68 | 32.37037 | 1.2333 | 29.280701 | 30.25925 | 4.0833333 | ||
| Std Dev | 13.06 | 13.02113 | 16.769183 | 15.80309 |
*Included in worst-case analysis.
Patient data was broken down by baseline Risser stage, with the purpose of evaluating how baseline Risser stage affected the outcomes at end of growth. This is shown in Table 2. For the highest risk curves at end of growth, Risser 0-1, 45% of them corrected, 38% were maintained, and 17% progressed. Of those curves that progressed, 3 of them progressed to surgical threshold, representing 5% of the Risser 0-1 groups. The average baseline Cobb angle for this group was 34°±14, the average end-of-growth Cobb angle was 31°±17. Their average starting age was 11 years, 5 months, with an average total treatment time of 2 years, 11 months. In those Risser 0-1 curves that obtained correction, the average correction was 11°.
Table 2.
Evaluation of patients’ data by baseline Risser stage.
| Baseline Risser (N) | % Correction (N) | % Stabilization (N) | % Progression (N) |
|---|---|---|---|
| 0(23) | 43(10) | 30(7) | 26(6) |
| 1(32) | 47(15) | 44(14) | 9(3) |
| 2(17) | 53(9) | 35(6) | 12(2) |
| 3(13) | 62(8) | 38(5) | 0 (0) |
Baseline curves at Risser 2 averaged 31°±10, and 26°±15 at end-of-growth. Among baseline Risser 2 curves, 53% achieved an average correction of 13°, while 35% were maintained at ±5°, and 12% progressed beyond 5°. Of those that progressed, 1 curve progressed beyond surgical threshold (50°), while the other had already reached surgical threshold at baseline.
Patients were also grouped according to menarche status. All patients who were premenarchial at treatment initiation (a total of 29) were either Risser 0 or 1. Among these patients, 41% of them achieved a curve correction (13 of 29), 38% of them (11 of 29) maintained their curvatures, and 21% of them progressed more than ≥6° (6 of 29). There were an additional 9 patients with a Risser 1 at baseline. These patients started menses within 7 months prior to the start of treatment.
The SOSORT Guidelines also recommend grouping patients based upon their baseline Cobb angle, as well as their ending Cobb angle. This is shown in Table 3. When examining curves first treated between 10-19°, 71% of these patients (5 of 7) achieved a correction of 6° or more, while the remaining 2 (29%) progressed by more than 5°. Neither of these cases increased to surgical threshold (>50°). For patients initiating the described rehabilitation treatment between 20-29°, 19 of 33 patients (58%) achieved a correction by the end of growth, while 12 of the 33 (36%) maintained their curvatures to within ±5°. The remaining 2 of the 33 patients saw their curves progress 6° or more; but not beyond surgical threshold. In the 30-39° starting range, 37% of patients had corrections in their curves (7 of 19), 31.5% of patients had their curves progress more than 6° (6 of 19), and 31.5% of patients (6 of 19) remained ±5° at end of growth. A total of 15 patients began treatment with curves between 40-49°. Of these, 8 patients had curve correction, 6 patients had curve stabilization of ±5°, and 1 patient had her curve increase over 6°. This patient was subsequently referred for surgical consultation. Finally, 10 patients initially presented with curves above surgical threshold (>50°). These patients had elected to forego previously recommended surgical intervention. A total of 4 of these patients had curve corrections, 5 of them maintained their curves, and 1 had a curve progression.
Table 3.
Patients grouped upon their baseline Cobb angle, as per the SOSORT Guidelines recommend.
| Range | N | %Imp | %Prog | Stabil |
|---|---|---|---|---|
| 10-19° | 7 | 71 | 29 | 0 |
| 20-29° | 33 | 58 | 6 | 36 |
| 30-39° | 19 | 37 | 31.5 | 31.5 |
| 40-49° | 15 | 53 | 7 | 40 |
| >50° | 10 | 40 | 10 | 50 |
| 84* |
*Number includes both curves in patients with a double curve pattern.
The data were also classified according to each curve pattern: thoracic, lumbar, thoracolumbar, and double major. These data are shown in Table 4. There were 17 total patients with a thoracolumbar curve pattern. In this group, 11 patients achieved correction, 5 maintained their curves, and 1 progressed. For the 16 patients with thoracic curves, 11 were corrected, while 5 were maintained. None of these patients progressed. In lumbar curves, 1 patient achieved correction, while the remaining 2 patients stabilized their curves. For patients with a double major curve pattern, 8 out of 24 patients achieved correction, 11 patients were maintained, and 5 patients progressed.
Table 4.
Data classified according to each curve pattern.
| Curve type | Cohort | %Correction | %Stabilization | %Progression |
|---|---|---|---|---|
| TL | 17 | 64.7(11) | 29.4(5) | 5.9(1) |
| T | 16 | 68.8(11) | 31.3(5) | 0 |
| L | 3 | 33.3(1) | 66.7(2) | 0 |
| D | 24 | 33.3(8) | 45.8(11) | 20.8(5) |
| Cohort | 60 | 51.7 | 38.3 | 10 |
TL, thoracolumbar; T, thoracic; L, lumbar; D, double major.
When totaling the number of cases who started below 50° and progressed to beyond 50°, 2 patients saw their curves progress to that point. The remaining patients with curves beyond 50° at end of treatment had already reached 50° by the time treatment was initiated. Of these, half of them achieved a curve reduction to below 50° by the end of follow-up. A total of 5 of these patients were referred for surgical intervention due to lack correction.
There were 3 patients in this cohort that did not follow up through Risser 3/4. Of these, 1 had curve progression, 1 patient achieved correction, and 1 was maintained. As part of a worst-case analysis scenario, if it is assumed that all 3 patients had failed in their treatment by the time they reached skeletal maturity, our total failure rate would be 13%. This would include these 3 patients, plus 5 other patients who had at least one curve progress 6° or more at final follow-up. These 5 patients who progressed that had follow-ups at skeletal maturity were recommended for surgical intervention.
Discussion
This study is the largest study to evaluate the impact of chiropractic rehabilitation treatment on adolescent idiopathic scoliosis when managed from onset through skeletal maturity. However, there are some important points that need to be discussed. First, the extent of chiropractic manipulation used in these cases was de-emphasized in both clinics. Although the decision whether to provide manipulation on a given day was a clinical decision made at the time by the rendering provider, only 40% of all patients received manipulation at any point throughout their one- or two-week therapy. We feel this is an important distinction to make, as many patients and providers equate chiropractic care with spinal manipulation, and this is not always the case as this study demonstrates.
While selection bias is always a concern in retrospective study designs, our goal was to evaluate everyone who had completed this process and fit the criteria. However, an important additional parameter in future studies will be to provide a quantification on home care compliance, since this may well affect the outcome of exercise-based protocols such as that illustrated in this study.
The SOSORT and SRS criteria indicate that adolescent, skeletally immature, high-risk patients should be braced if their curves exceed 25°.14 In the present study, patients selected for inclusion had either declined the bracing treatment option by another provider, or were given the option for concurrent therapy with the exercises described herein, but decided to forego bracing as a component of treatment. Hence, patients proceeded with rehabilitation, only after informing them of the standard of care and their decision to decline that aspect of treatment. Future studies should look at the combination of the chiropractic rehabilitation described in this study with part- or full-time rigid bracing. Although no control group was used in this study, the criteria laid out by the BrAIST study and the SOSORT/SRS committees clearly define what outcomes are considered important. Therefore, using these known and accepted parameters allowed us to determine if these results were clinically meaningful and statistically significant. It will also allow various types of exercise-based therapies to compare methodologies so that newer exercise theories and treatment approaches can evolve.
Conclusions
This retrospective chart review demonstrated that 90% of patients who participated in a chiropractic rehabilitation treatment for adolescent idiopathic scoliosis, and were followed through at least the end of growth, achieved a curve correction or stabilization. For those patients achieving correction, their average correction was 12.75°. All but 2 patients who were followed all the way through skeletal maturity whose curves started below 50° were able to keep their curves below 50°. Worst-case analysis showed a failure rate of 13%. These patients went on to surgical consultation. Further prospective trials are needed to verify and strengthen the results of this study. The current study design does not allow for extrapolation of results to other cases.
References
- 1.Lonstein JE. AIS. Lancet. 1994;344:1407-12. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447-55. [PubMed] [Google Scholar]
- 3.Weiss HR. The method of Katharina Schroth – history, principles and current development. Scoliosis 2011;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Romano M, Negrini A, Parzini S, et al. SEAS (Scientific Exercises Approach to Scoliosis): a modern and effective evidence based approach to physiotherapic specific scoliosis exercises. Scoliosis 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss HR, Negrini S, Hawes MC, et al. Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment – SOSORT consensus paper 2005. Scoliosis Spinal Disord 2006;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reamy BV, Slakey JB. AIS: review and current concepts. Am Fam Phys 2001;64:111-6. [PubMed] [Google Scholar]
- 7.Romano M, Negrini S. Manual therapy as a conservative treatment for adolescent idiopathic scoliosis: a systematic review. Scoliosis 2008;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monticone M, Ambrosini E, Cazzaniga D, et al. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J 2014;23:1204-14. [DOI] [PubMed] [Google Scholar]
- 9.Kuru T, Yeldan I, Dereli EE, et al. The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil 2016;30:181-90. [DOI] [PubMed] [Google Scholar]
- 10.Schreiber S, Parent EC, Moez EK, et al. The effect of Schroth exercises added to the standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis-an assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner”. Scoliosis 2015;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dovorany D, Morningstar MW, Stitzel C, Siddiqui A. Results of chiropractic scoliosis rehabilitation treatment at two years post-skeletal maturity in identical female twins. J Bodyw Mov Ther 2015;19:592-6. [DOI] [PubMed] [Google Scholar]
- 12.Morningstar M. Four-year follow-up of a patient undergoing chiropractic rehabilitation for adolescent idiopathic scoliosis. J Pediatr Matern Family Health 2011;16:54-8. [Google Scholar]
- 13.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Negrini S, Hresko TM, O’Brien JP, Price N, SOSORT Boards and SRS Non-Operative Committee Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non–operative management committee. Scoliosis 2015;10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morningstar MW. Outcomes for adult scoliosis patients receiving chiropractic rehabilitation: a 24-month retrospective analysis. J Chiropr Med 2011;10:179-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berdishevsky H, Lebel VA, Bettany-Saltikov J, et al. Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Scoliosis Spinal Disord 2016;11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]



